Rethinking Network Design: Turning Informed Choice into a Reality

By Dr. Matthew Resnick, MD, MPH | Chief Medical Officer, Senior Vice President, Health Plan Business, Embold Health
In healthcare, more has long been equated with better: more providers in-network, more choices for members, more access points. It’s an idea that feels right on the surface. But as anyone who’s ever tried to choose a doctor knows, more doesn’t always mean better, and it certainly doesn’t mean easier.
We’re challenging that assumption. We're rethinking what it means to design a network, not by how expansive it is, but by how effective, transparent, and member-centered it can be.
The Illusion of Choice
Health plans have historically touted broad networks as a benefit. After all, more providers should lead to lower costs and greater satisfaction, right? The reality is more complicated.
Across virtually every health plan network, there is multifold variation in provider performance, even within the same health system, specialty, or geographic area. As consolidation has swept across each and every healthcare market, providers and facilities join hospitals, hospitals join health systems, and the result is dramatic variation in quality among providers and facilities practicing under the same ‘banner.’
Offering choice is unquestionably attractive – both for members and for plan sponsors – however, choice is only valuable insofar as it is informed by credible information. Most people aren’t trained to evaluate providers by outcomes, adherence to evidence-based guidelines, or resource use. They rely on word-of-mouth, online reviews, or health plan directories - none of which are purpose-built to meaningfully differentiate between high- and low-performing providers.
We can do better. By leveraging objective, validated performance data, we can illuminate the differences that matter - so people can choose doctors who consistently deliver high-value, high-quality care.
Because information alone isn’t enough. To truly transform decision-making, we need to incentivize better choices.
From Rewards to Rational Networks
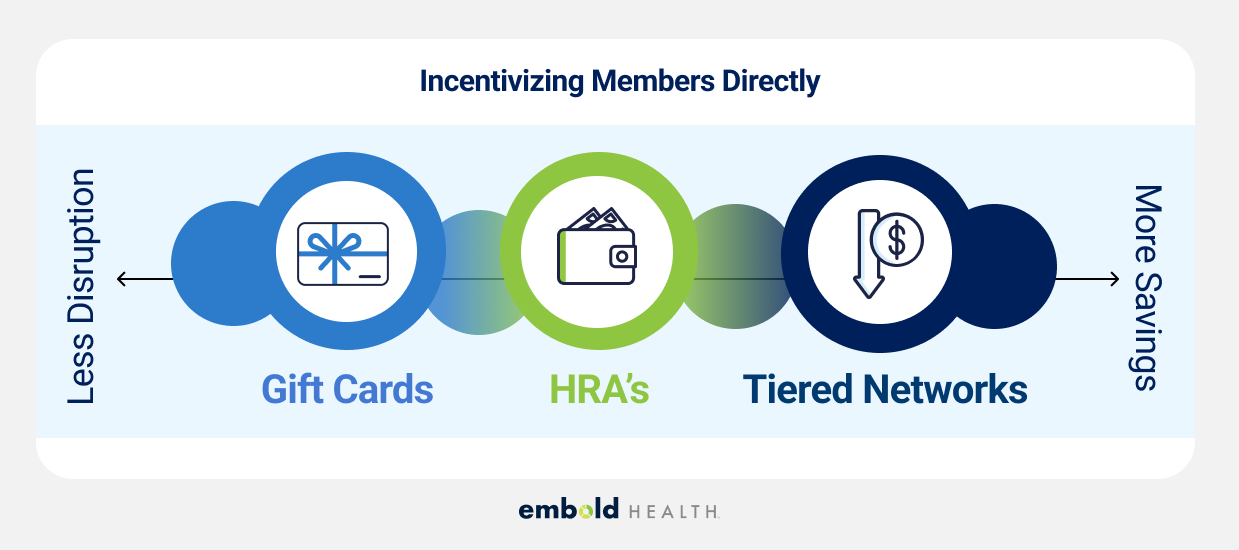
There’s a powerful continuum of interventions available to health plans and employers looking to support choice with information and incentives. It starts simply: reward members for engaging with tools that guide them to better care. A gift card for selecting a high-performing provider might seem small, but it's meaningful at scale, and it is a simple incentive that everybody understands and values.
Then we can begin layering in benefit design. Tiered cost-sharing, where top-tier providers offer lower out-of-pocket costs, nudges members toward better decisions. Even modest financial signals can guide people away from a family member’s referral and toward a high-performing provider backed by credible and transparent quality data.
Eventually, we get to network design - where the very structure of a network is shaped not by negotiated prices alone, but also by provider quality. As discussed in a prior blog post, the industry has historically believed that cost and quality were at odds. We believe the opposite – that we have an opportunity to optimize networks on both quality and cost, delivering significant value to health plans, plan sponsors, and employees along the axes of cost of care and outcome improvement.
The Role of Transparency and Collaboration
Of course, you can’t build a network like this in a vacuum. Provider engagement is essential.
One of Embold’s core beliefs is that transparency should be a two-way street. We provide physicians with clear, comprehensible performance data, often for the first time in their careers. During my tenure as a surgeon at a large academic medical center, I rarely received objective insights into how the care I delivered compared to my peers.
By opening that black box and giving providers a path to improve, we avoid turning quality measurement into a game of winners and losers. It’s not about excluding providers; it’s about offering an invitation for improvement and empowering them to rise to the challenge.
We also recognize the risk of solving one problem only to create another. Narrowing networks to only the highest performers could, if done blindly, lead to access bottlenecks. Our approach balances rigor with realism, ensuring members can still get timely, high-quality care without overwhelming the providers who deliver it.

A Smarter Future for Networks
Healthcare is shifting. Rising costs and economic pressure are forcing employers and health plans to look for smarter solutions — ones that don’t just cut costs but simultaneously improve quality of care and outcomes.
Network design, when approached with nuance, data, and transparency, offers a powerful lever. It allows us to replace the illusion of choice with informed, incentivized, and accessible options. And in doing so, it helps members, providers, and plans alike move toward a better, more sustainable healthcare system.
Because at the end of the day, a network isn’t about who’s in it — it’s about getting patients to providers who are delivering the right care, at the right time, for the right reasons.
.avif)









