Request a demo
See if we can improve the health outcomes of your employees. It only takes 15 minutes.
Generative AI is reshaping healthcare navigation with real-time, personalized insights that empower better care decisions and lower costs.

Finding the right doctor, understanding where to go for care, and making sense of benefits shouldn't be hard. Yet for most employees and health plan members, healthcare navigation is confusing, slow, and disconnected from their daily lives. Even with digital tools and support lines, many still end up in the wrong place — or nowhere at all.
Generative AI is changing this. Not as a replacement for clinical insights, but as a guide to meet people where they are, offer timely support, and avoid low-quality care decisions. It is reshaping healthcare navigation by stepping in where outdated tools fall short, bringing clarity, speed, and smarter choices to moments that matter most.
Letters. Portals. Emails. App reminders. Most member portals operate using a "pull" system that expects people to know what they're looking for, when they need it, and where to find it — a significant burden in an already confusing system. These platforms are:
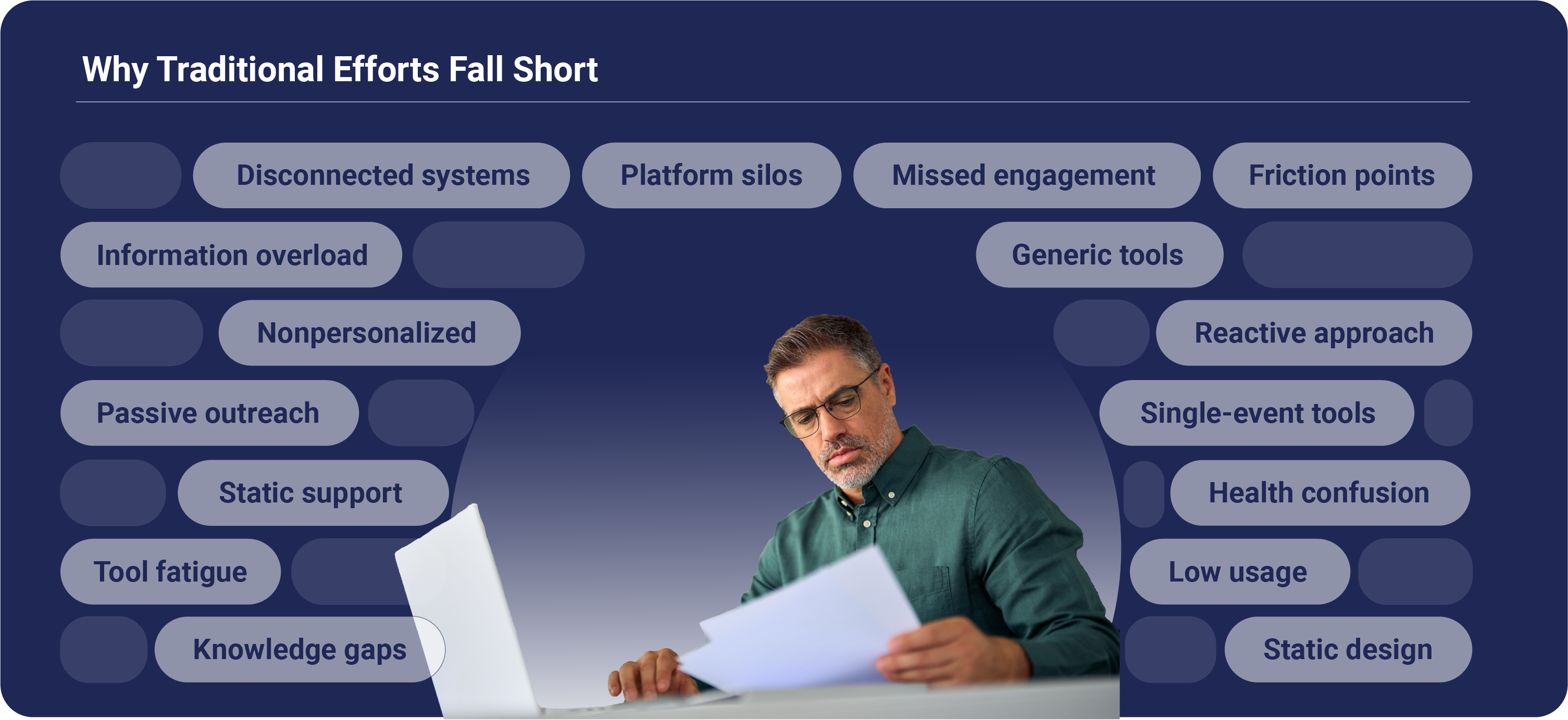
The evidence? Fewer than 10% of members use traditional portals or tools, even after significant investment on behalf of health plans and employers. This disconnect has measurable consequences that impact both healthcare outcomes and overall spend:
To lower costs and improve outcomes, the smartest investment isn’t in more point solutions, it’s in better ways to guide members to high-quality care.
Outside healthcare, consumers are transitioning away from traditional search to intelligent agents like ChatGPT for quick, personalized, and conversational answers. And it’s working: AI-driven personalization has been shown to increase customer satisfaction by 10–20% and reduce service costs by up to 30%.
Generative AI is particularly powerful because of its potential to address the core limitation of "pull" systems: the assumption that members know what they need and when to seek it. Generative AI assistants don't wait for members to ask for help — they engage in real-time during the moments that matter most, across familiar channels with intelligent, personalized guidance.
This goes far beyond answering "Who's in my network?" Instead, it helps members navigate harder questions like:
They’re not simple bots, they combine multiple data streams — benefits structure, provider quality scores, and individual preferences — to deliver personalized recommendations that feel tailored and trustworthy. This level of personalization is what drives the behavior change that health plans and employers need for sustainable improvements.

Generative AI tools like Embold’s Virtual Assistant (EVA) are transforming how people navigate healthcare by offering personalized guidance at the exact moment decisions are being made.
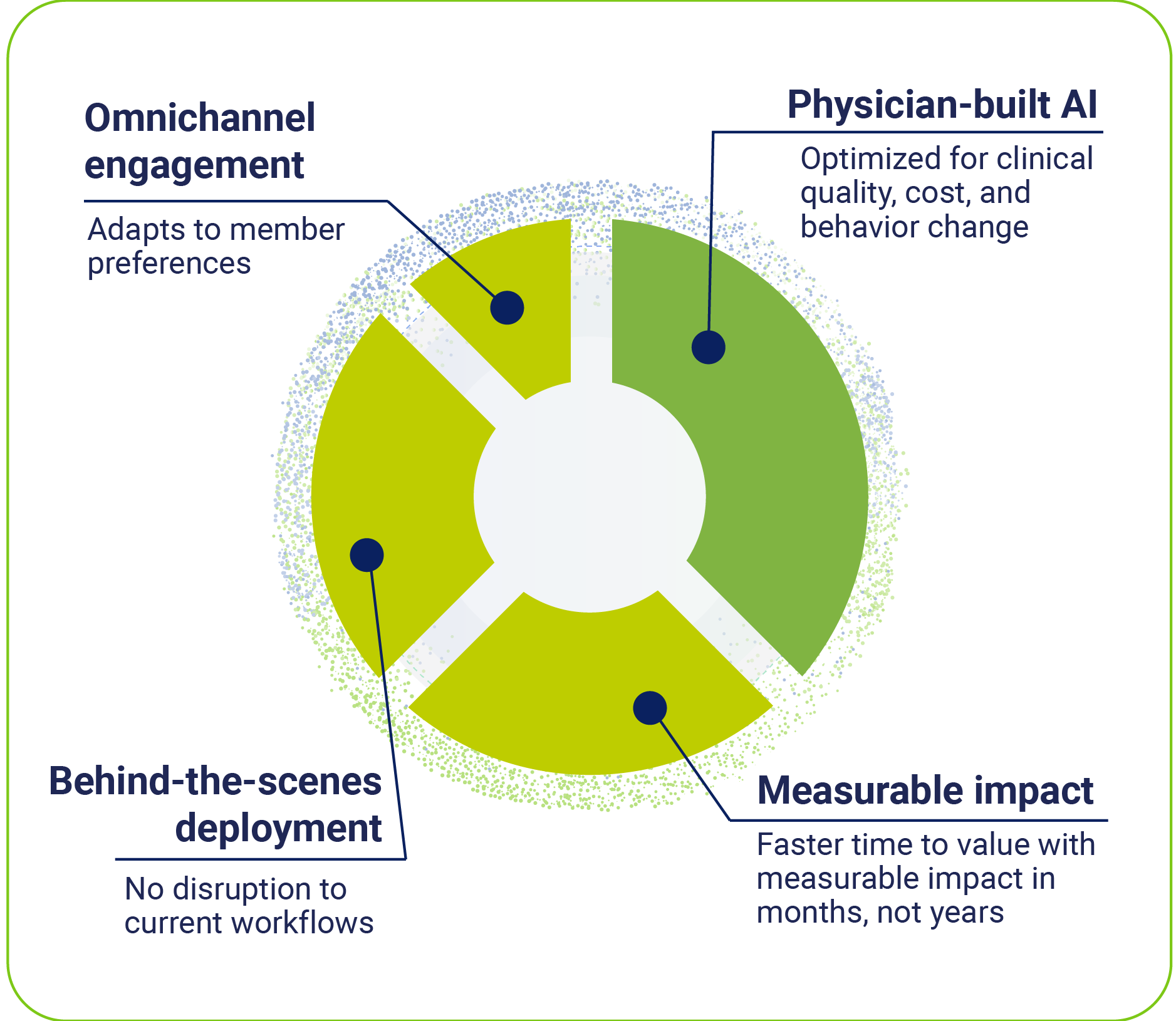
Unlike traditional tools, EVA offers real-time, omnichannel support across multiple touchpoints — text messages, email, benefits portals, and workplace tools like Microsoft Teams. EVA is neutral, evidence-based, and grounded in clinical quality. That's because the technology was developed with a physician-led foundation that prioritized outcomes over transactions.
After integrating Embold's Virtual Assistant, one national employer saw immediate results, including:
Generative AI is ushering in a new era in healthcare navigation — more intelligent, adaptive, and member-centered. While traditional digital engagement has plateaued and costs continue to rise, this shift from passive search to dynamic guidance represents one of the most important advances in member experience and cost containment. In fact, patients with higher engagement levels incur 8% lower healthcare costs in the first year and 21% lower costs in the subsequent six months.
These tools are finally delivering on the long-promised goal of personalization at scale, meeting members in the moment they need support and guiding smarter care decisions. Embold Health’s e-book, Beyond the Portal, showcases how transformation is reshaping member engagement and creating measurable impact. This level of personalization is what drives the behavior change that health plans and employers need to see sustainable improvements in both outcomes and costs.
The technology is proven, the results are measurable, and the opportunity for health plans and employers is immediate.
See if we can improve the health outcomes of your employees. It only takes 15 minutes.